Chronic health conditions can cause many problems, and one of the more unpleasant ones is cold feet. Your feet feel cold all the time. And it’s not just your imagination—poor blood flow due to an uncontrolled medical condition really can make your feet colder than they should be. Thankfully, you can take steps to warm up your cold feet. This blog post will discuss some causes of cold feet and what you can do about them.
What are the causes of cold feet?
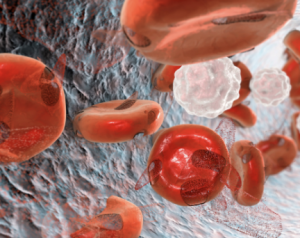
Anemia
Anemia is when you do not have enough healthy red blood cells to carry adequate oxygen to your body’s tissues. This can cause weakness, fatigue, dizziness, pale skin, and cold hands and feet. Several things, including blood loss, lack of iron in your diet, or an underlying medical condition, can cause anemia. It is important to talk to your doctor if you think you might have anemia.
What are the different types of anemia?
There are many types of anemia, each with its own cause.
Vitamin deficiency anemia
You can develop this type of anemia if you don’t have enough vitamin B12 or folic acid in your diet. Vitamin B12 and folic acid help the body make new red blood cells.
Aplastic anemia
When your bone marrow does not produce enough new red blood cells. Certain medications, cancers, or autoimmune diseases can cause aplastic anemia.
Sickle cell anemia
This is a type of hemoglobinopathy, which means there is a problem with the structure of hemoglobin. Sickle cell anemia can cause pain, organ damage, and even death.
Anemia of chronic disease: This type of anemia happens when you have a chronic illness like cancer, HIV/AIDS, rheumatoid arthritis, or kidney disease.
Diabetes
According to the Centers for Disease Control and Prevention (CDC), more than 30 million people in the United States—or 9.4% of the population—have diabetes. Of those 30 million, about 23 million have been diagnosed with diabetes, while the remaining 7 million are living with undiagnosed diabetes. (Centers for Disease Control and Prevention, 2017)

There are three types of diabetes:
Type 1 Diabetes
Type 1 diabetes—sometimes called juvenile diabetes or insulin-dependent diabetes—is usually diagnosed in children, teens, or young adults. In type 1 diabetes, the body does not produce insulin. Insulin is a hormone that helps the body break down and use glucose for energy. People with type 1 diabetes must take daily insulin injections or use an insulin pump to control their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes can occur at any age, although it is most often diagnosed in middle-aged or older adults. In type 2 diabetes, the body does not produce enough insulin or does not use insulin properly. When this happens, glucose cannot get into the cells and builds up in the bloodstream. Type 2 diabetes is often treated with diet, exercise, and medication. However, some people may need to take insulin injections as well.
Gestational Diabetes
Gestational diabetes happens when your pancreas can’t make enough insulin to handle the added hormone production during pregnancy. This causes your glucose to get too high. If you have gestational diabetes, your baby is getting too much sugar. This could lead to your baby being born early, too big, or having low blood sugar after birth. You may also have a higher chance of having premature labor, stillbirth, or c-section.
Eye, kidney, and circulation problems can occur if diabetes is not controlled. Circulation problems can sometimes cause poor blood flow in the legs and feet. As a result, a person with diabetes can develop leg and foot issues, such as chronic pain, swelling, sores, and cold feet.
Peripheral Arterial Disease
Approximately 6.5 million people aged 40 and older in the United States have PAD. Both men and women are affected by PAD; however, African Americans have an increased risk of PAD. Hispanics may have slightly higher PAD rates, similar to non-Hispanic white people. (Centers for Disease Control and Prevention, 2022).
Peripheral arterial disease (PAD) is a condition that occurs when your arteries are narrow or blocked, which limits blood flow to your extremities. While PAD is most common in the legs, it can also cause cold feet. When blood flow is restricted, your feet may not get enough oxygen and nutrients, which can cause them to feel cold. Poor blood flow can lead to other problems, such as pain, numbness, and ulcers.

What are the symptoms of a cold foot?
- Mild, throbbing pain in your feet and toes
- Feet that take longer to warm up if you’re exposed to cold temperatures
- Feet that are a different color (pale, red, blue, or purple) than the rest of your body
- Cold feet during specific hours of the day, like at night
How to Treat Cold Feet
- Wear socks made from natural fibers like wool or cotton. These materials will help to insulate your feet and keep them warm.
- Wear shoes that fit well and don’t constrict your feet. Tight shoes can restrict blood flow and make your feet even colder.
- Exercise regularly. Exercise helps improve blood circulation throughout your body, including to your feet.
- Soak your feet in warm water for 10-15 minutes each day. This will help improve blood flow to your feet and make them feel warmer.
- Massage your feet each day with lotion or oil. This will also help improve blood circulation to your feet.
- Avoid smoking cigarettes. Smoking constricts blood vessels and makes it harder for blood to circulate properly throughout your body—including your feet!
- Check your blood sugar levels regularly and manage them according to your doctor’s recommendations. Good glycemic control is essential for preventing diabetes complications like poor blood flow.
When should I call the doctor?
If you have cold feet, don’t ignore it. If your feet seem cold all the time, it’s time to call us, as this may indicate that you have a more serious issue. We will perform a comprehensive exam, which includes asking you about your symptoms, current lifestyle, and risk factors. After your evaluation, we may recommend additional testing, like an x-ray or an ultrasound of the affected leg and foot. Finally, depending on the cause and complexity of your pain, we may prescribe lifestyle changes, medications, or a procedure.
Our patient care does not stop after you walk out of our facilities. We schedule follow-up appointments that help us to evaluate the results and recovery. Our friendly physicians and staff members will also provide you with answers to your concerns or questions after every appointment, diagnostic test, and medical procedure. We strive to offer all our patients the best possible results, allowing them to get back on their feet quickly.
References
Centers for Disease Control and Prevention. (n.d.). Peripheral Arterial Disease (PAD) | cdc.gov. CDC. Retrieved November 26, 2022, from https://www.cdc.gov/heartdisease/PAD.htm
Centers for Disease Control and Prevention. (2017, July 18). New CDC report: More than 100 million Americans have diabetes or prediabetes | CDC Online Newsroom. CDC. Retrieved November 12, 2022, from https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html
Diabetic.Org. (n.d.). Is Type 2 Diabetes Genetic? Diabetic.org. Retrieved November 12, 2022, from https://www.diabetic.org/is-type-2-diabetes-genetic/