Pelvic Venous Congestion Treatment
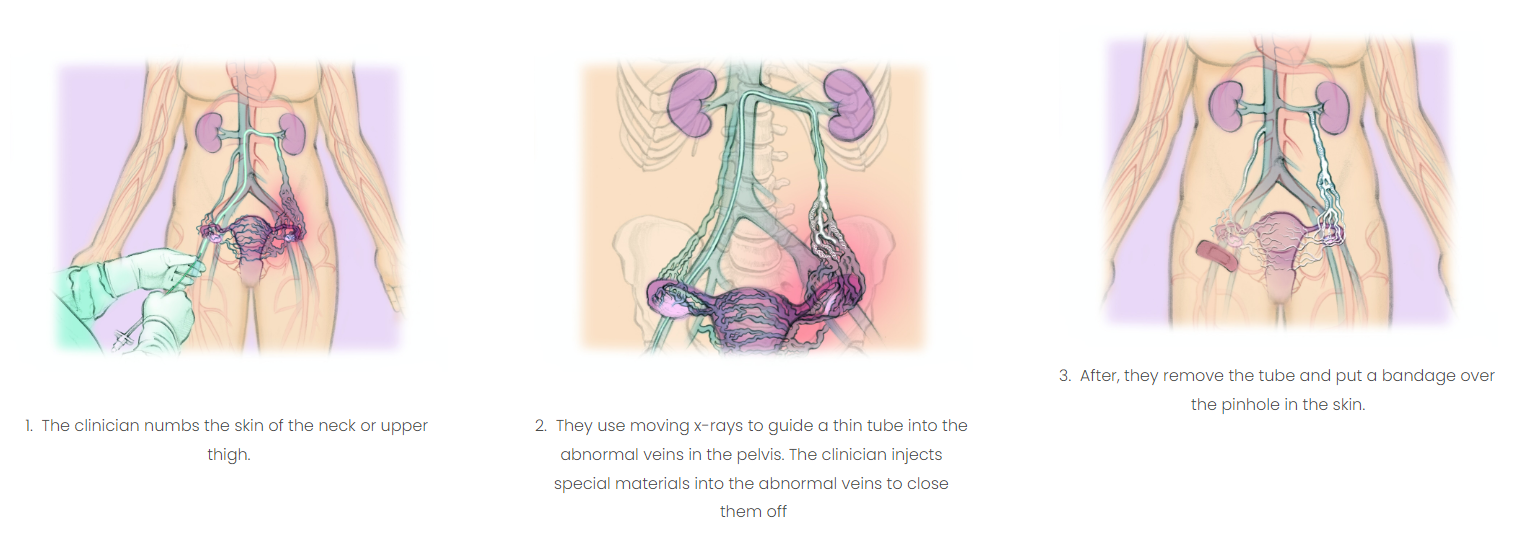
Embolization is performed to relieve pelvic venous congestion, using a catheter to access the problematic ovarian veins. It is a painless outpatient procedure that requires no major incisions.
Your health is our priority.
Contact us today.
Embolization for Pelvic Venous Congestion
*Illustration Credit to The Interventional Institute.
Ovarian/Gonadal vein embolization starts when your vascular specialist will inject sclerosing agents into the varicose veins through a catheter. Next, the surgeon attaches small metal plugs or coils to prevent blood flow into the veins. This prevents reflux in the ovarian/gonadal veins and eases pressure within the engorged veins.
Embolization is an outpatient procedure that provides access to the problematic ovarian veins using a catheter. The procedure is painless and requires no major incisions. The surgeon will embolize each problematic vein (blocking blood flow) with vascular plugs or coils. Doing so seals off the varicose veins, diverting blood flow to healthy veins. The surgeon will also deliver sclerosing medication to lower the pressure in the pelvic veins and relieve the pain. Once blood can flow smoothly through healthy veins in the pelvic and labial area, the pain disappears. Patients can usually return to work and light activities the day following the procedure and see a full recovery in about one week. At least 7 in 10 women who undergo the procedure report significant symptomatic relief. This procedure is usually performed by a trained interventional radiologist on an outpatient basis.
WHAT ARE THE RISKS?
- Gonadal vein embolization is generally a safe procedure when done by a specialist.
- Blocking the unhealthy veins can irritate them, which can cause temporary pain and fever.
- The unhealthy veins can come back or symptoms do not improve in 1 in 10 women.
- The special material used to block the vein can go somewhere else in the body in 1-2 in 100 women.
This can cause symptoms or no symptoms depending on where the material ends up. - Other rare complications include bleeding or infection at the wound site.
- The procedure DOES NOT affect the menstrual cycle or fertility. It does use radiation.
Even though the radiation dose is very small, it could harm the ovaries.
Why Monterey Bay Vascular?
At Monterey Bay Vascular, we offer coordinated care to prevent, diagnose, and treat vascular disease.
We understand, everyone deserves to live a long, happy life. Vascular disease may lead to limb loss and other life-threatening conditions such as pulmonary embolism. Our licensed vascular surgeon uses state-of-the-art tools and technology to tackle all problems related to your vascular system. Thanks to our vast wealth of experience, we also work with our patients to develop a unique solution that fits your needs. Contact us today to learn more about the vascular treatments we offer and schedule an appointment today!