Peripheral Artery Disease
Individuals suffering from peripheral arterial disease, or PAD, are at a higher risk of coronary artery disease, stroke, or heart attack. If left untreated, PAD can lead to wounds, gangrene, and limb amputation. While the pain primarily occurs in the legs, it can also be felt in other parts of the body, including the arms, stomach, hip, head, and kidneys.
Your health is our priority.
Contact us today.
What Is Peripheral Artery Disease (PAD)?
30% to 40% of Americans who report leg pain while walking have PAD.
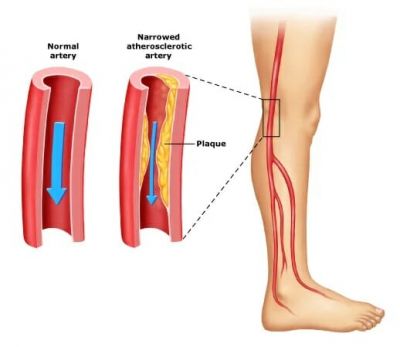
The most common symptom associated with
peripheral arterial disease is leg pain when walking or exercising. This condition is also referred to as claudication. Fat and cholesterol build up on the artery walls can impede healthy blood flow. When this happens, your muscles are not able to receive oxygen and, therefore, can start to ache and cramp, especially during exercise. Symptoms that are associated with peripheral arterial disease are listed below.
Peripheral Arterial Disease - Symptoms
- Non-healing wounds or ulcers
- Weakness or numbness in your legs
- Coldness feet (one foot may be colder than the other one)
- Pain in your feet or toes while you are resting
- Muscle cramps during exercise
- Slower toenails growth
- Change in the color of your feet
- Erectile dysfunction in men
- Weak pulse in your feet or legs
- Developing shiny skin on your legs
- Pain in your arms, especially when performing manual
- Thinning skin on your legs
As peripheral arterial disease progresses, you may experience pain even when you are lying down. The pain can even become intense enough to disrupt your sleep.
Resting your legs by hanging them at the edge of your bed or a brief walk can stimulate blood flow.
What Causes Peripheral Arterial Disease?
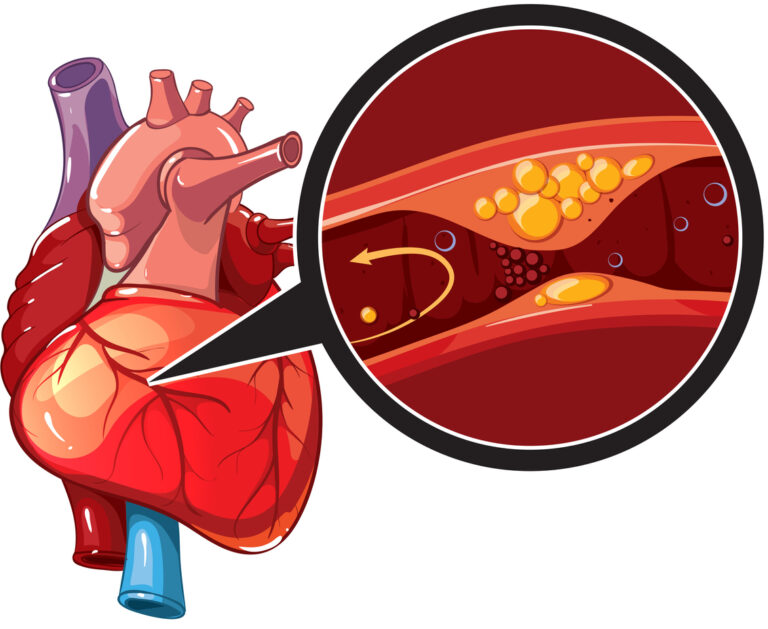
Atherosclerosis, the most common cause of PAD, develops when excessive plaque buildup is present in the artery wall. The plaque is usually made up of cholesterol and fat buildup. The condition starts when the plaque builds enough to narrow an artery, restricting blood flow. Next, the plaque may become inflamed or brittle, causing a rapture that triggers a blood clot to form. The blood clot will narrow the artery further or block it entirely. Blockages in the arteries can lead to life-threatening conditions. For instance, if the carotid artery is blocked, it can cause a stroke. If the blockages remain in the legs’ peripheral arteries, it can lead to pain, skin discoloration, sores, and difficulty in walking. In extreme cases, complete loss of circulation to the feet and legs can lead to gangrene and limb loss. If you do not have atherosclerosis, the following conditions may also cause Peripheral Artery Disease.
Controllable Risk Factors of PAD
Over 8 million Americans suffer from Peripheral Arterial Disease
Smoking
The most common symptom associated with peripheral arterial disease is leg pain when walking or exercising. This condition is also referred to as claudication. Fat and cholesterol build up on the artery walls can impede healthy blood flow. When this happens, your muscles are not able to receive oxygen and, therefore, can start to ache and cramp, especially during exercise. Symptoms that are associated with peripheral arterial disease are listed below.
Lack of Exercise
Lack of exercise can also increase your risk of PAD. If you are suffering from PAD, establishing a regular exercise regiment will significantly improve your painful symptoms. Regular workouts improve blood flow and boosts overall health by regulating blood sugar and blood pressure. It also lowers cholesterol and reduce plaque buildup.
High Cholesterol,
High Blood Pressure
& Diabetes
Diabetics are at high risk of PAD if they have consistently high blood sugar. High blood glucose is connected to plaque buildup in the arteries. Controlling Type 2 diabetes through the proper diet, exercise, and medication helps in reducing PAD risks. Patients diagnosed with high blood pressure and high cholesterol are also at increased risks of PAD. Maintaining a healthy diet and exercise can help reduce blood pressure and cholesterol, which is key to reducing PAD risks.
1 in 3 People with heart disease will develop Peripheral Arterial Disease.
Diagnosing PAD
At Monterey Bay Vascular, we offer comprehensive diagnosis and develop customized treatments for peripheral arterial disease. We understand that no two patients’ conditions are similar. Our full-service vascular lab provides state-of-the-art tests ensure that we address each patient case quickly and accurately. Our team has extensive experience in our specialized field and use advanced tools to achieve limb-saving results even in the most challenging cases.
At Monterey Bay Vascular, we also use ultrasound-guided testing to determine whether a specific vein or artery is blocked or open. We utilize two main ultrasound tests. The first method is an Arterial Doppler ultrasound utilized to locate areas with blockages or reduced blood flow in your arteries. An ultrasound technician uses a handheld device that sends sound waves through the arteries to measure how fast blood flows.
The second method is the Segmental Doppler pressure testing that checks various parts of the legs for blocked or narrowed arteries. The procedure is similar to the ABI test, but the ultrasound device will amplify the sound of blood flow, making it easy to measure blood pressure. After the ultrasound, you’ll receive a thorough consultation. The doctor will recommend the most effective treatment option to optimize lower extremity blood flow.
Ankle-brachial index (ABI test) and Toe-brachial index (TBI) helps diagnose PAD. This test compares the blood pressure in your arm with the blood pressure in your ankle and toes. The doctor uses a pressure cuff coupled with an ultrasound device. Sometimes, the doctor may request that you walk on a treadmill while they take the readings before and immediately after the exercise. These diagnostic tests will help the doctor to capture the severity of potential narrowed arteries.
To help diagnose PAD, the doctor will conduct a thorough review of your medical history. The doctor will also want to learn about your symptoms, personal health history, risk factors, and family health history. The doctor will ask you several questions regarding your medical conditions, such as diabetes, heart disease, and kidney disease. They will also ask you if you have experienced pain or cramps in your leg while walking or exercising. The doctor will also inquire about your family history of PAD and other heart diseases. You will also discuss smoking habits, both current and past.
After gathering this information, the doctor will proceed to perform a detailed physical examination. The process involves checking for weak pulses in your feet and reviewing blood flow levels in your diagnostic ultrasounds. The doctor will also check for any problems on your legs, such as sores, swelling, and pale skin.
After reviewing all diagnostic testing, alongside your physical exam, our team will recommend the best course of treatment and educate you on treatment options.
Sometimes, more detailed diagnostics are needed. If that is the case, you may find that your doctor may order an Angiography (Diagnostic Angiogram) or a Magnetic resonance Angiography (MRA).
An angiography (diagnostic angiogram) is a minimally invasive test that helps to visualize and diagnose blockages inside veins and arteries. During this test, the doctor will insert a thin tube, called a catheter, that injects a special dye. The dye will project blood vessels on an X-ray. As the dye is introduced to the arteries and veins, fluoroscopy imaging captures the detailed images to see the extent of the blockages in the arteries.
An MRA is conducted to examine the structure of the arteries in your body. An MRA is a type of MRI that uses powerful magnetic fields, radio waves and a computer to evaluate your blood vessels and help physicians detect abnormalities.
Why Monterey Bay Vascular?
At Monterey Bay Vascular, we offer coordinated care to prevent, diagnose, and treat vascular disease.
We understand, everyone deserves to live a long, happy life. Vascular disease may lead to limb loss and other life-threatening conditions such as pulmonary embolism. Our licensed vascular surgeon uses state-of-the-art tools and technology to tackle all problems related to your vascular system. Thanks to our vast wealth of experience, we also work with our patients to develop a unique solution that fits your needs. Contact us today to learn more about the vascular treatments we offer and schedule an appointment today!