Pelvic Venous Congestion Syndrome
Varicose veins are most common on the feet and legs, but they can also occur in the pelvis causing chronic pelvic pain in women. This condition is known as pelvic congestion syndrome (PCS) or ovarian vein reflux.
Your health is our priority.
Contact us today.
What Is Pelvic Venous Congestion Syndrome?
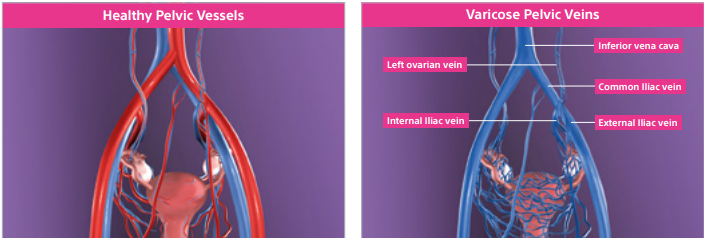
Pelvic Venous Congestion Syndrome (PCS) is essentially varicose veins in the pelvis.
It is the cause of chronic pelvic pain in approximately 13-14% of women.
Research has shown that 1 in every 7 women, and 1 in 5 women who have had children, have varicose veins that come from the pelvis.
Varicose veins are most commonly seen in the legs and are caused by valve malfunction (valves in the veins do not work properly and they do not stop blood from flowing backwards). Veins become less elastic, bulky and enlarged. When this happens to the pelvic veins, visible varicose veins emerge in the pelvic region and the pressure often causes severe pain and discomfort. The varicose veins in the pelvis surround the ovary and can also push on the bladder and rectum.
Symptoms of Pelvic Venous Congestion
Pelvic venous congestion syndrome is most commonly experienced for the first time during or following pregnancy. It is characterized as a heavy aching feeling that may get worse as pregnancy progresses. Typically, you feel the pain on the left side only. PCS pain is usually worse during the evenings.
Additional symptoms are listed below:
- Low back pain
- Pelvic pain, vaginal pain, groin pain, leg pain, or back pain
- Dilated leg or pelvic varices (varicose veins)
- Painful intercourse or bleeding after intercourse
- Unexplained urinary urgency, frequency, or sensation
of incomplete bladder emptying
- Heavy and/or painful periods
- Pain with ovulation
- Leg swelling and symptoms after superficial vein treatments
- Feeling of physical anxiety in the chest when
one does not feel mentally anxious - Migraine headaches
Diagnosing Pelvic Venous Congestion
There are a few different methods that are used at Monterey Bay Vascular to diagnose pelvic congestion.
Pelvic venous congestion syndrome can be difficult to diagnose because while many women experience pelvic pain, it is not always the result of having Pelvic venous congestion.
Aside from PCS, some individuals are diagnosed with May-Thurner Syndrome (MTS) or
Gonadal Vein Insufficiency (also known as Ovarian Vein Insufficieny).
Our physician will be able to diagnosis and treat you for either PCS, MTS and Gonadal Vein Insufficiency.

Diagnostic Options
Our state-of-art diagnostic testing allows for an accurate, timely diagnosis.
Congested veins in the pelvis and lower abdomen can be diagnosed with an ultrasound. This diagnostic test helps the vascular surgeon to visualize backward blood flow and identify enlarged veins in your pelvic region.
Abdominal and pelvic CT and MRI scans help help the vascular surgeon visualize suspected backward blood flow in more detail. A CT or MRI of the pelvis or abdomen may be ordered in addition to an ultrasound to help the doctor get a clearer picture of your veins.
A pelvic venography is an X-ray imaging technique used to take images of veins in the pelvis. It’s the most definitive, minimally invasive screening technique when checking for pelvic venous congestion syndrome. During a pelvic venography, a catheter is inserted into a vein through your neck or groin. Then, it is guided into the veins in the ovary. An iodine-based dye is used to obtain detailed images of the pelvis. This is a same-day procedure that does not require general anesthesia. From start to finish a venography takes no more than one hour.
After the images have been taken, the catheter is removed. The doctor will then apply slight pressure on the puncture area to stop bleeding. You will be discharged 1 to 4 hours later. A pelvic venography may also be used as a treatment method in conjunction with pelvic embolization.
Treatments for
Pelvic Venous Congestion Syndrome (PCS)
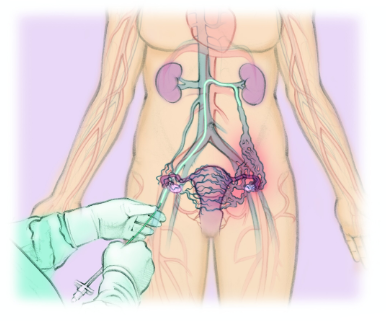
*Illustration Credit to The Interventional Institute.
Reach Out to Our Team
Why Monterey Bay Vascular?
At Monterey Bay Vascular, we offer coordinated care to prevent, diagnose, and treat vascular disease.
We understand, everyone deserves to live a long, happy life. Vascular disease may lead to limb loss and other life-threatening conditions such as pulmonary embolism. Our licensed vascular surgeon uses state-of-the-art tools and technology to tackle all problems related to your vascular system. Thanks to our vast wealth of experience, we also work with our patients to develop a unique solution that fits your needs. Contact us today to learn more about the vascular treatments we offer and schedule an appointment today!